what are the implications of having fiber-optic cable to everyone’s home?
Keywords
Disc herniation; Classical micro discectomy; Endoscopic epidural light amplification by stimulated emission of radiation disc decompression
Introduction
More than than half of adults complain of depression dorsum hurting at least one time in their lifetime [1,two]. Low back hurting is a mutual cause of admission to the infirmary [2,three]. Acute low dorsum pain in most patients heals inside the first 2 months without treatment; however, for few patients, it becomes chronic despite medical treatment [three-five]. Open up surgery and spinal instrumentation have been the traditional treatment modalities for discogenic pain for many years. The clinical success rate in the early postoperative period after open up surgery is 95% to 98% and recurrence rate is 2% to v% [6,seven]. Inadequate physiotherapy secondary to the healing of epidural injuries leading to leg and depression back pain and secondary to fibrosis in the post-operative menstruation decreases surgical success rate to 80% in subsequent follow-ups [7,8].
In classical micro discectomy applications (CMA), the paravertebral muscles are peeled off from where they attach to the spinous procedure. Therefore, there is pain attributable to musculus trauma in the early post-operative period. This increases the need for post-operative analgesics.
Cheng et al. argues that thermal annuloplasty is reliable and effective in the treatment of carefully selected patients with single-level discogenic lumbar hurting [ix]. Endoscopic epidural light amplification by stimulated emission of radiation decompression (EELD) enables herniated disc ablation with laser or forceps, similar to interference gain from the sacral hiatus. This process is typically accompanied past a holmium: yttrium-aluminum-garnet (Ho: YAG) laser [ten,11]. Many articles on EELD accept reported that the Visual Counterpart Calibration (VAS) is an important tool of measurement in the cess of hurting [12-14]. Herniated intervertebral disc is associated with radiculopathy and low back pain in patients [12]. Ruetten et al. treated chronic back and leg pain syndrome with epiduroscopy-guided Ho: YAG laser intervention (north=93) and reported 45.9% positive results postoperatively [11].
In this written report, we aimed to compare the effects of CMA and EELD on the VAS values and complications in patients with discogenic low back and leg pain owing to protrusion, extrusion, sequestration, or jutting.
Materials and Methods
After the approval from the local ethics committee of Gazi Yaşargil Educational activity and Research Infirmary of the University of Health Sciences in Turkey, the data from the patients who applied to the neurosurgery outpatient clinic betwixt January 2013 and January 2016 were screened, and the patients with leg hurting more severe than low back pain (assessed via the Lasegue's sign, Bragard's sign, femoral nerve stretch test, Naffziger'south exam, and Cram test positive), with disc protrusion, extrusion, sequestration, or bulging in their MRI, who underwent CMA (due north=79) or EELD (due north=54), were retrospectively evaluated.
Application of CMA and EELD
All patients who were treated with CMA and EELD were informed about the procedure and complications before the process. The patients were too informed about VAS evaluation and written informed consent was obtained from the patients.
Age, gender, neurological examination findings, level of disc with bulging, extrusion, sequestration, or protrusion (via clinical and MRI findings), and VAS were used to evaluate radiculopathic pain level matching the disc level, and the arising complications were recorded. It was seen that cases with no signal loss (black disk) in MRI imaging of patients with clinical findings (sagittal T1A and T2A as well as axial T2A), with >10 mm of disc height and bulging, extrusion, sequestration, protrusion or annular rupture that could cause radiculopathy, were evaluated for the procedure.
The exclusion criteria
• Disc superlative of <10 mm on MRI
• Previous lumbar surgery
• Leg and lumbar pain with non-intraspinal disc origin (intraspinal tumors, epidural abscesses and hematomas, nerve infection, facet syndrome, and spondylolisthesis)
• Leg and lumbar pain with non-extraspinal disc origin (pelvic and femoral tumors, sacroiliac dysfunction, piriformis syndrome, sacroiliitis and seronegative spondyloarthropathies, non-sciatic nerve entrapment neuropathies in pelvis, myofascial pain syndromes, trochanteric bursitis, hip osteoarthritis, peroneal nervus compression, and maralgia paresthetica), and systemic infection or infection at the intervention area.
The inclusion criteria
• ASA Group I-Three
• Aged between 30 and 85years
• Disc herniation and (bulging, extrusion, sequestration, or protrusion) matching this level
• Disc height of >x mm
• Pain symptoms for at least iii-6 months and no response to medical and conservative treatment methods such equally concrete therapy (behavioural methods, psychosocial regulations, and exercise programs) (VAS score of ≥ 5),
• Receiving sensory examination at areas matching L3, L4, L5, and S1 nerve roots and checked for pain by involvement examination at areas matching L3, L4, L5, and S1 nerve roots as well every bit 1 or more nervus root involvement in clinical exam (consistent with radiological findings) and complaints consistent with radiculopathy
• Leg pain more than severe than low dorsum hurting (assessed via the Lasegue's sign, Bragard'south sign, femoral nerve stretch test, Naffziger's test, and Cram exam positive).
Before the study, information technology was confirmed that non-steroidal antiinflammatory, salicylic acid, and similar drugs that could lead to bleeding coagulation disorder were discontinued at the appropriate time, and combination of tramadol and paracetamol was started for the patients for whom analgesics were discontinued. It was seen that oral tramadol and paracetamol and thiocolchicoside were used postoperatively in the first 24 hours, and the drugs causing bleeding coagulation disorder were restarted at the advisable time. Pre-operative low back and leg VAS values were recorded.
It was seen that routine blood tests of the patients were confirmed before the procedure and the patients were accustomed for the procedure according to the standard fasting protocol on the day of application. The patients were taken to the operating room on the day of the process, intravenous vascular access was established, and isotonic sodium chloride solution was started. I hour before the procedure, 1 g cefazolin was intravenously administered. The patients were taken to the operating tabular array in the prone position and the lower abdomen was left empty to prevent venous fullness. All applications were performed under sterile conditions and with C-arm fluoroscopy. It was seen that CMA applications were fabricated under spinal or full general anaesthesia, whereas EELD applications were made nether only infiltration anaesthesia and appropriate dose of sedoanalgesia.
Based on the patient files, we observed that the CMA process was performed as follows: On the mean solar day of the functioning, the patients were taken to the operating table and an intravenous catheter was inserted from the back of the hand and started from SF 100 ml/h.
After the pre-op preparation, spinal anaesthesia or full general anaesthesia in the supine position was induced, and the patients were intubated and moved to the operating table in the prone disc position. The procedure started after the necessary sterilization and roofing.
After the cutaneous and subcutaneous incision, the blunt autopsy revealed the muscles. The Taylor spinal retractor was placed in the operation surface area, and upper and lower hemi partial laminectomy was performed using microscopic imaging. The excision of the ligamentum flavum was performed.
Using root retractors, the root was retracted to the medial side. Ligament excision was performed with scalpel number 15. Displacement was performed with the disc forceps (Figure 1). Post-obit haemostasis, the tissues were closed anatomically and the performance was concluded.
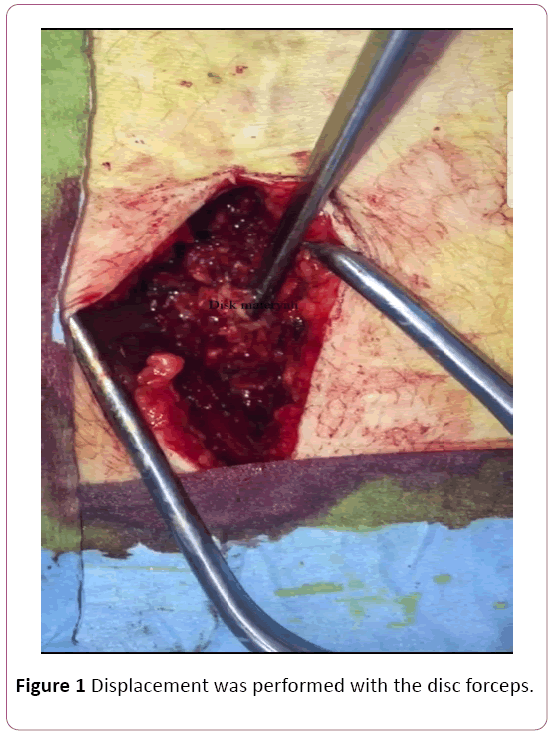
Figure ane: Deportation was performed with the disc forceps.
Based on the patient files, we observed that the EELD procedure was performed as follows: On the day of the functioning, the patients were taken to the operating tabular array and an intravenous catheter was inserted from the dorsum of the paw and started from SF 100 ml/h. The patients were placed in the prone position, and a silicone pillow was placed under the abdomen to flatten lumbar lordosis and facilitate the intervention. The intervention surface area was readied for sterilization and local amazement was practical using 2% lidocaine; 5-10 mm skin incision was made on the sacral hiatus, a 17-judge Tuohy needle was entered into the sacrum, and a wire guide was placed. The dilatator was rotated over the wire guide and the layers were dilated. A steerable 3 mm video-guided catheter and a cobweb Li Ho: YAG laser were implanted. Lateral image and needle placement (at the lesser of the target disc, in the posterior longitudinal ligament) were confirmed with fluoroscopy and epiduroscopy and with the help of a video image (Figure 2) (anterior epidural space). Information technology was seen that anterior epidurogram was performed by giving 1-2 ml contrast agent and the pathology was outlined. Adhesiolysis immune localization and anatomical appearance of the pathology. Bulging was reduced with 2.5 Westward (0.v J, v Hz) increments using posterior longitudinal ligament (PLL) Ho: YAG light amplification by stimulated emission of radiation. First, the fibre optic cable video was inserted into PLL (through the pigsty in the PLL) under the herniated intervertebral disc, and the decompression of the herniated disc was started with Ho: YAG laser 8 W (0.8 J, 10 Hz). It was understood that the nerve root decompression of the ruptured disc was later decompressed past epiduroscopic confirmation. The functioning notes revealed that when the procedure was completed, the video was removed and the incision in the sacral hiatus was sutured.
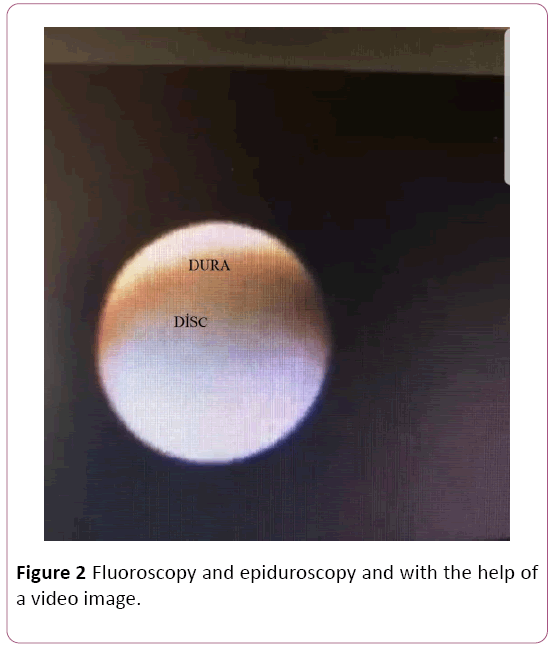
Figure 2: Fluoroscopy and epiduroscopy and with the help of a video image.
The patients were taken to the post-operative care room afterward the procedure. The patients were monitored for one hour and neurological examinations were made. The patients were then taken to the neurosurgery service. The VAS values of the patients were recorded at week 1, calendar month 1, month 6, year 1, and twelvemonth ii after the procedure. The efficacy of the procedure was evaluated past comparison the pre-op VAS values of the patients with the values at the calendar week i, month 1, month vi, year 1, and twelvemonth two. All arising complications were recorded.
Statistical analysis
In this study, all statistical calculations were evaluated with the SPSS version 11.five for the Windows parcel programme. The Shapiro-Wilk exam was used to bank check normality. The evaluation of the commonly distributed data was washed via parametric tests. The categorical data were defined equally n (%). Comparing of the unremarkably distributed data was washed with I-Sample T test, and the information were presented as mean (± standard divergence). A P value of <0.05 was considered statistically significant for all data.
Results
Patient data with respect to age, duration of operation, elapsing of complaint, gender, level of intervention, presence of pre-operative and post-operative neuropathy, and image of disc in MRI are presented in Tabular array 1.
| Variables | CMA (n=79) | EELD (n=54) | p-value | |
|---|---|---|---|---|
| Age (Year) | 47.99 ± 13.57 | 45.5 ± 12.03 | 0.079 | |
| Complaint time (Day) | 95.29 ± 51.07 | 96.38 ± 49.09 | 0.340 | |
| Gender (Male/Famale) | 51% (64.vi)-28% (35.4) | 36% (56.3)-28% (43.viii) | 0.610 | |
| Level | Fifty3-four | 12% (fifteen.19) | 9% (xiv.one) | 0.563 |
| L4-5 | 46% (58.22) | 38% (59.4) | 0.056 | |
| L5-Southward1 | 21% (26.59) | 17% (26.vi) | 0.062 | |
| Preoperative neuropathy (Yes/No) | 0% (0)-0% (0) | 0% (0)-0% (0) | 1 | |
| Postoperative (Yep/No) | 0% (0)-0% (0) | 0% (0)-0% (0) | i | |
| Disk condition | protrusion | 38% (48.10) | 41% (64.1) | 0.089 |
| extruded | 18% (22.79) | 8% (12.5) | 0.025 | |
| jutting | 7% (8.86) | 15% (23.4) | 0.037 | |
| sequestered | 16% (20.26) | 0% (0) | <0.001 | |
Table 1: Demographic data of CMA and EELD patients (Mean ± SD and due north%).
There was no statistical difference between the groups except for MRI images. Although the ratio of extruded and sequestered discs was higher in the CMA grouping, bulging was more frequent in the EELD group.
The comparison of the VAS values is given in Table 2. There was no statistically significant divergence between the CMA and EELD groups in terms of pre-operative VAS values.
| Variables | CMA (n=79) | EELD (northward=54) | p-value |
|---|---|---|---|
| Preoperative VAS value | 6.44 ± 1.23 | 7.55 ± 0.94 | 0.576 |
| Postal service-operative 1. calendar week VAS value | iii.38 ± 0.88 | 2.34 ± 0.79 | 0.012 |
| Post-operative 1. calendar month VAS value | three.01 ± 0.16 | 2.56 ± 0.97 | 0.458 |
| Mail-operative 6. month VAS value | 2.24 ± 0.68 | 2.55 ± 0.71 | 0.032 |
| Post-operative ane. year VAS value | 2.22 ± 0.34 | 2.59 ± 0.89 | 0.014 |
| Post-operative 2. year VAS value | i.78 ± 0.12 | 2.33 ± 0.fourscore | 0.028 |
Table 2: Comparison of preoperative, post-operative 1st week, 1st month, 6th month, 1st yr and twond year VAS values of CMA and EELD patients (Mean ± SD).
There was a statistically significant departure betwixt the VAS values recorded post-operatively at week ane because the VAS values were significantly higher in the CMA grouping than those in the EELD group (Table two).
The VAS values recorded pre-operatively at month 1 were significantly higher in the CMA group than those in the EELD group (Table 2).
When values recorded at calendar month 6, year 1, and year ii were compared, it was found that the VAS values were significantly lower in the CMA grouping than in the EELD group (Table 2).
The comparison of the frequency of post-operative complications is presented in Tabular array 3. When the patients were compared in terms of depression back pain, the frequency of low back pain was significantly higher in the CMA group than in the EELD group (Table 3).
| Variables | CMA (n=79) | EELD (due north=54) | p-value | |
|---|---|---|---|---|
| Spinal instability hurting | Aye/No | 21%26.59-58%73.41 | 11%17.2-53%82.4 | 0.068 |
| Radiculopathy | Yes/No | 36%45.57-43%54.43 | 23%35.9-41%64.1 | 0.076 |
| Depression dorsum pain | Yeah/No | 71%89.88-8%10.12 | 32%50-32%l | 0.004 |
| Hipoindent disc | Yeah/No | 34%43.03-43%54.43 | 24%17.5-40%62.5 | 0.063 |
| Discitis | Yes/No | 0%0-79%100 | 2%3.1-62%96.9 | 0.038 |
| Hematoma | Yes/No | ii%2.53-77%97.47 | 0%0-64%100 | 0.068 |
| Mail-operative fibrosis | Yeah/No | 5%6.32-72%95.68 | two%3.1-62%91.9 | 0.076 |
Tabular array 3: Comparison of postoperative complications in CMA and EELD patients (n %).
When the patients were compared in terms of discitis, it was found that the distribution of discitis was significantly lower in the CMA group than in the EELD group (Table 3).
Discussion
Depression back hurting affects approximately lxxx% of the population at some point in their lives and is i of the nigh common causes of referral to healthcare institutions [15,16]. Information technology is as well a very significant health problem economically because of the workforce loss it causes and the expenditures for diagnosis and treatment; 80%–xc% of patients suffering from pain are healed with conservative handling, just ten% of patients develop chronic low back pain [17,18]. The recurrence charge per unit during the 5-year follow-upwards is 60% for the patients who have been relieved of pain.
The nigh of import structures in the etiology of low dorsum pain are intervertebral discs, facet joints, and sacroiliac joints. The idea that intervertebral discs have their own innervations and may cause intrinsic pain was first presented by Inman and Saunders in 1947 and reported in detail by Bogduk and Groen et al. [xix-21].
Many surgical techniques, such every bit discectomy by laminectomy, micro discectomy, spinal fusion, and recently, disc prostheses, accept been developed in the handling of lumbar disc affliction. The success charge per unit subsequently classic discectomy was reported to exist 95% to 98% in the short term and the recurrence gamble of disc herniation was reported to be 2% to half-dozen% [7,15,22]. In the long term, the success rate decreases to eighty% owing to the recurrence of disc herniation, epidural fibrosis, increment of spondylosis findings, and development of instability.
In another written report, in add-on to the magnification and illumination of the surgical microscope, Scoville et al. reduced mail-operative complications owing to incision past achieving smaller incisions and less muscle retraction using the retractor systems they developed [23]. In discectomy with classical microsurgery, the paraspinal muscles are separated from the tendinous insertions with the subperiosteal arroyo and retracted from the spinous processes. Paraspinal muscles are rich in proprioceptors and are injured owing to local ischemia when retracted [24]. There is a correlation between postoperative pain and denervation and retraction ischemia [25].
Spengler et al. studied 54 patients and found that patients who were very satisfied after open discectomy showed expert results and had higher scores in the pre-operative period according to the scoring arrangement created by neurological, psychological, sciatic stretching symptoms, and imaging studies [26-29]. In our study, we besides performed discectomy with open microsurgery under a microscope and establish that patients' VAS values decreased in the 1st calendar week.
Park et al. showed that EELD is a adept handling option in carefully selected patients with disc-originated low dorsum and radicular pain [thirty]. In our report, the effectiveness of EELD was too demonstrated. Nosotros constitute that the VAS values decreased in the 1st week.
Jo et al. showed that 85% of patients were satisfied with the EELD procedure [31]. Nosotros constitute that the VAS values decreased in the 1st week. However, the VAS values measured at week 1, months 1 and 6, and years 1 and 2 were <5 for both CMA and EELD patients. The VAS values recorded at week ane and calendar month 1 were significantly lower in the EELD group, and we think that this was because of the paraspinal muscles not retracting. However, the VAS values recorded at month 6 and years 1 and 2 were found to be significantly lower in the CMA grouping. This suggests that CMA is more effective in the long term.
Comparison of the complexity frequencies is shown in Table iii. Depression back hurting was significantly more frequent in the CMA group than in the EELD group. This was likewise thought to be owing to retraction in the paraspinal muscles. Conversely, discitis was significantly higher in the EELD group. It was idea that this could be owing to heat generation by the light amplification by stimulated emission of radiation.
Conclusion
In conclusion, when discectomy by microsurgery and EELD were compared, it was found that the VAS values were <v in both groups in the long and curt term, but low back pain was significantly lower in the EELD group, whereas frequency of discitis was college. The finding that total economic expenditure in the EELD grouping being much higher and the procedure taking longer suggests that CMA is a cheaper method that tin be safely used in these patients and has results like to those obtained by EELD.
References
- Izci Y, Apaydin O, Ozdem T, Cerrahoglu M (2003) The bony malformations of lumbosacral junction and sacrum: Case reports and literature review. Tohoku J Exp Med 201: 277-281.
- Izci Y, Taskaynatan MA (2004) Direction of lower back pain in immature Turkish recruits. Mil Med 169: 824-828.
- Andersson GB (1999) Epidemiological features of chronic depression-back hurting. Lancet 354: 581-585.
- Nachemson AL (1992) Newest knowledge of low back pain: A critical await. Clin Orthop 279: 8-20.
- Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, et al. (2005) Clinical significance of built lumbosacral malformations in immature male population with prolonged depression back pain. Spine xxx: 210-213.
- Erdine S (2002) Interventional techniques in pain direction. Ankem sixteen: 182-184.
- Erdine S, Ozyalcin NS, Cimen A (2005) Percutaneous lumber nucleoplasty. Agri 17: 17-22.
- Gangi A, Dietemann JL, Mortazavi R, Pfleger D, Kauff C, et al. (1998) CT-guided interventional procedures for pain direction in the lumbosacral spine. RadioGraphics 18(3): 621-633.
- Cheng J, Zheng W, Wang H, Li C, Wang J, et al. (2014) Postero-lateral transforaminal selective endoscopic diskectomy with thermal annuloplasty for discogenic low back pain: A prospective observational study. Spine 39: 60-65.
- Ruetten Southward, Meyer O, Godolias G (2002) Awarding of holmium: YAG light amplification by stimulated emission of radiation in epiduroscopy: Extended practicabilities in the handling of chronic back pain syndrome. J Clin Laser Med Surg twenty: 203-206.
- Ruetten S, Meyer O, Godolias G (2003) Endoscopic surgery of the lumbar epidural space (epiduroscopy): Results of therapeutic intervention in 93 patients. Minim Invasive Neurosurg 46:one-4.
- Lee SH, Lee SH, Lim KT (2016) Trans-sacral epiduroscopic laser decompression for symptomatic lumbar disc herniation: A preliminary instance series. Photomed Laser Surg 34: 121-129.
- Jo D, Finch PM, Oh J (2016) Epiduroscopic laser neural decompression for removal of L2–l3 Disc herniation in a patient with symptoms suggestive of L5 nerve root involvement. Pain Med 17: 1386-1388.
- Jo DH, Yang HJ (2013) The survey of the patient received the epiduroscopic light amplification by stimulated emission of radiation neural decompression. Korean J Pain 26: 27-31.
- Andreula C, Muto Chiliad, Leonardi Thou (2004) Interventional spinal procedures. Eur J Radiol fifty: 112-119.
- Peng B, Hao J, Hou S, Wu W, Jiang D, et al. (2006) Possible pathogenesis of painful intervertebral disc degeneration. Spine 31(5): 560-566.
- Singh V, Derby R (2006) Percutanous lumbar disc decompression. Hurting Phycian 9: 139-146.
- Enthoven P, Skargren Eastward, Oberg B (2004) Clinical course in patients seeking master automobile efor dorsum and neck hurting: A prospective 5-year follow-up of outcome and health intendance consumption with subgroup analysis. Spine 29: 2458-2465.
- Bogduk NI, Windsor Yard, Inglis AD (1988) The innervation of the cervical intervertebral discs. Spine 13(one): 2-8.
- Groen 1000, Baljet B, Drukker J (1990) The nerves and nerve plexuses of the human vertebral column. Am J Anat 188(3): 282-296.
- Inman VT, Saunders JB (1947) Anatomicophysiological aspects of injuries to the intervertebral disc. J Bone Joint surg 29(ii): 461-475.
- Rasouli MR, Rahimi-Movaghar Five, Shokraneh F, Moradi-Lakeh G, Chou R (2014) Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev iv: 010328.
- Ulus A (2009) Lomber Diskektomi ve Laminektomi icin TÃÆ'¼p Esliginde Mikrocerrahi. TÃÆ'¼rk NÃÆ'¶rosirÃÆ'¼rji Dergis 19: 195-200.
- Brock M, Kunkel P, Papavero L (2008) Lumbar microdiscectomy: Subperiosteal versus transmuscular approach and influence on the early on postoperative analgesic consumption. Eur Spine J 17: 518-522.
- Christie SD, Song JK (2006) Minimally invasive lumbar discectomy and foraminotomy. Neurosurg Clin N Am 17: 459-466.
- Yuan H, Xu JB, Wang H (2007) The clinical results of microendoscopic discectomy and conventional (Love’s) discectomy. Chinese Periodical of Spine and Spinal Cord 17: 808-812.
- Hussein M, Abdeldayem A, Mattar M (2014) Surgical technique and effectiveness of micro-endoscopic discectomy for large uncontained lumbar disc herniations: a prospective, ran-domized, controlled study with 8 years of follow-upward. Eur Spine J 23: 1992-1999.
- Mu, X Wei J, Peifeng L (2015) What were the advantages of microendoscopicdiscectomy for lumbar disc herniation comparingwith open up discectomy: a meta-assay?. Int J Clin Exp 8: 17498-17506.
- Spengler DM, Ouellete EA, Battie Thousand, Zeh J (1990) Elective discectomy for herniation of lumbar disc. Boosted experience with an objective method. J Bone Joint Surg Am 72: 230-237.
- Park CH, Lee SH (2017) Endoscopic epidural decompression versus transforaminal epiduroskopic laser annuloplasty for lumbar disc herniation: A prospective randomized trial. Pain physician 20: 663-670.
- Jo DH, Kim ED, Oh HJ (2014) The comparison of the event of epiduroscopic laser neural decompression between FBSS or non. Korean J Pain 27: 63-67.
Source: https://www.aclr.com.es/clinical-research/retrospectively-analysis-of-the-effects-on-patients-visual-analogue-scale-values-and-complications-of-disc-decompression-performed.php?aid=23928
0 Response to "what are the implications of having fiber-optic cable to everyone’s home?"
Post a Comment